Lung Compliance
Lung compliance explained in video
Lung Compliance: The Ability to Stretch.

If you’ve been around respiratory care or pulmonary medicine any length of time, you are likely very familiar with the idea of both lung compliance and airways resistance. The concept of compliance is arguably the more complex of the two, and RTs everywhere seem to be enamored by a pursuit to confirm whether a patient has low lung compliance. Chances are, you too find yourself constantly questioning your patient’s lung compliance, but no worries because you are in good company.
The simplest way to conceptualize the idea of lung compliance is to think of compliance as the lung tissue’s ability to stretch overall. Think for instance about a rubber band. A tight (usually thicker) rubber band is more difficult to stretch and therefore snaps back with great force. A loose (usually thinner) rubber band is easier to stretch and has a weaker snap back. The concept of lung tissue compliance is not that much different than the basic concept of stretch and recoil. Yes, we are dealing with millions of tiny sac-like structures (alveoli) and not a rubber band. And, yes, these microscopic alveoli tend to share borders and some of their walls as the clusters begin to manifest from the respiratory bronchioles. But, other than the fact that alveoli are closely packed together and have an air fluid interface, they’re just tiny balloons right? Well, certainly the alveoli have very little in common with a balloon literally speaking, but figuratively, it seems helpful enough to simply think about the behavior of a balloon when thinking about compliance of alveoli.

Alveoli are an important part of the respiratory system whose function it is to exchange oxygen and carbon dioxide molecules to and from the bloodstream
I would be remised if it was not emphasized that each individual alveolus has its own individual compliance. This means that during inspiration, a cluster of alveoli may begin filling at different intervals and readily fill and expand together until a certain point at which certain alveoli in that cluster cease to expand while others continue. A good analogy might be if you are pushing against 2 people at the same time, but one weighs significantly less than the other. The lighter person would be easy to push over whereas the heavier person would take greater force to move. During mechanical ventilation, when flow is forced into the lung and intrapulmonary pressure is created, it is the alveoli’s resistance to expansion (ability to stretch) that causes the pressure to accumulate. Yes, the chest walls resistance to expansion also influences the pressure that is required, but we are concentrating on the alveoli for this discussion, remember?
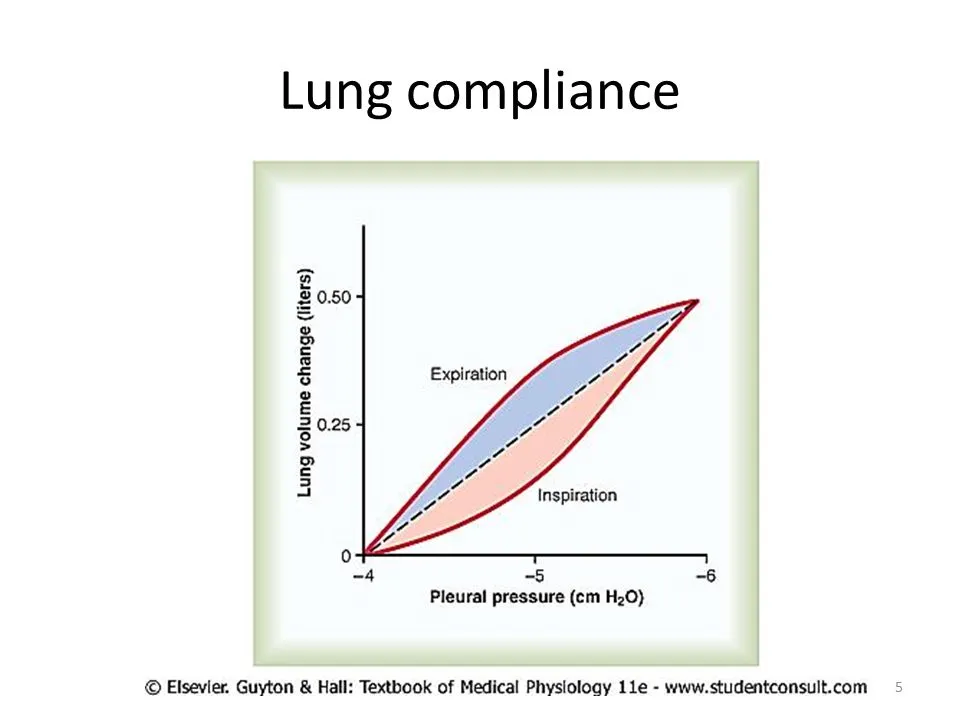
To oversimplify compliance as a general mathematical concept, you are comparing volume to pressure. Lung compliance is the amount of volume per unit pressure. The unit for compliance is usually given in liters or milliliters (vol) per centimeter of water (pressure). Think of it as the amount of volume that is produced for every 1 cmH2O applied. To further discuss the basics of static compliance versus dynamic compliance, one must revisit the math equations that renders the value for each – it’s not that bad, here’s the basic versions of each equation below:
Static compliance = tidal volume / (plateau pressure – PEEP)
CL static = (Vt ) / (Pplat – PEEP)
Dynamic compliance = tidal volume / (peak inspiratory pressure – PEEP)
CL dynamic = (Vt ) / (PIP – PEEP)
Remember, during mechanical ventilation, in order to manually acquire and/or estimate lung compliance, flows must not be excessive, and the patient should not be actively/spontaneously breathing during the measurement. Some ventilators allow a constant autogenerated compliance measure, but this is beyond the scope of this discussion.
Clinically, when a patient has lung disease that is diverse, individual alveoli may have highly variable critical opening pressures as well as inconstant critical closing pressures. Literally speaking, each alveolus requires a certain pressure to recruit, and alveoli that fully collapse at end-expiration (atelectasis) may require high pressures to be forced back open. Remember, a tight rubber band (or smaller balloon) is difficult to stretch but has a powerful recoil force. In fact, the reciprocal of lung compliance (ability to stretch) is elasticity (recoil force).
Compliance is inversely related to elasticity: CL = 1 / EL
Elasticity is inversely related to compliance: EL = 1 / CL
When considering lung compliance, it should be noted that the lung is situated within the sealed chest cavity, essentially surrounded by a stiff, bony thorax. Because the lung has a natural tendency toward collapse (passive recoil inward) and the thorax has a natural tendency toward expansion (passive recoil outward), the oppositional forces between the lung and thorax create a vacuum – our negative intrapleural pressure. Keep in mind, anytime that the normal relationship between lung tissue and thorax is altered, the means in which lung tissue expands and recoils is going to be altered.
Under normal spontaneous conditions, think Boyle’s Law, the lung fills with volume because the diaphragm contracts (descends) and creates more volume within the thorax creating a drop in intrapleural pressure.
The intrapleural pressure is already slightly negative but becomes more negative, tethering open the delicate lung units. Once the diaphragm relaxes and passively recoils (ascends), thoracic volume decreases, allowing the negative intrapleural pressure to become less negative, returning to its prior resting state, and the lung tissue passively recoils.
In summary, normally the lung fills with volume during inspiration as a result of pressure gradient changes, causing flow to enter the airway and alveoli; expiration occurs during passive recoil of the lung, allowing partial emptying of alveoli until the lungs return to their resting volume (aka. functional residual capacity). Compliance is a traditionally a concept to account for overall respiratory system compliance and measured during positive pressure ventilation. Therefore, most discussions typically center around that perspective.
Static compliance is the true measure of lung distensibility as this measurement is acquired when the lung is at tidal volume but during a short breath hold. Because there is no flow to account for, airways resistance is not a consideration. Dynamic compliance, on the other hand, is more of a constant estimate of volume per unit pressure but can be influenced by airways resistance. During a dynamic compliance measurement, total volume during inspiration (aka. tidal volume) is compared to the highest-pressure during inspiration (aka. peak pressure). Here’s the equations again for comparison:
Static compliance = tidal volume / (plateau pressure – PEEP)
CL static = (Vt ) / (Pplat – PEEP)
Dynamic compliance = tidal volume / (peak inspiratory pressure – PEEP)
CL dynamic = (Vt ) / (PIP – PEEP)
Patient ‘X’ is a 45 year old Asian male in volume control mode, set Vt: 450mls, set PEEP: 5 cmH2O, peak inspiratory pressure (PIP): 22 cmH2O, plateau pressure: 16 cmH2O
If your patient continues in a volume-targeted mode of ventilation with no spontaneous efforts, you will simply need to acquire the values required for the above equations in order to calculate both static and dynamic compliance. You should note that dynamic compliance will be lower than static, and static is the true compliance measure since airways resistance is taken out of consideration for the static compliance calculation.
CL static = (Vt ) / (Pplat – PEEP)
= 450 / 16 – 5
= 450 / 11
= 41 mls/cmH2O
CL dynamic = (Vt ) / (PIP – PEEP)
= 450 / 22 = 5
= 450 / 17
= 26.5 mls/cmH2O
As a reminder, compliance is usually only measured during a volume-targeted mode of ventilation where flow is constant (peak flow is set). For plateau pressure to be acquired, an inspiratory breath hold is required. Static compliance is arguable the more important of the two since flow is not a factor, therefore airways resistance is not a factor. A compliance estimate in any mode of ventilation can be a valuable metric to allow insight into the volume delivered per unit of pressure applied.
In closing, if you can estimate how much volume can be produced in the lung for each unit of pressure applied, then you can appreciate your patient’s lung compliance. As lung compliance decreases, the volume per unit pressure will decrease, and as lung compliance increases, the more volume will result for each unit of pressure applied. The patient with so-called “stiff” lungs, will require higher ventilating pressures to attain adequate ventilating volumes. For those with stiff lungs, you should constantly consider whether the patient could simply tolerate lower volumes. The consideration of lung recruitment techniques and allowance of permissive hypercapnia should also be part of your ongoing contemplations. Finally, if lung compliance is extremely low, it may be best to adopt a pressure-targeted mode of ventilation and therefore be able to exactly control the amount of pressure applied to the lung.
source:
https://respiratorycram.com/lung-compliance-the-ability-to-stretch/
Comments section

Maximous
Perfect
